In the spring of 2020, the world shut down. Like so many families, we were navigating lockdowns, remote school, and the general uncertainty that came with the start of the pandemic. My son, a high school junior at the time, was part of his school’s cross-country and track teams. He was also in the marching band—active, lean, and always on the go. At 5’10” and around 118 pounds, he was a classic distance runner build. Slim, but seemingly healthy.
But then, something shifted.
The Diagnosis
A couple of months into lockdown, my son came to me and quietly admitted he hadn’t been feeling well. He was experiencing bouts of diarrhea and told me he had lost a few pounds—he was down to 108 pounds. When I looked at him closely, I noticed he looked pale. Really pale. We booked an appointment with his pediatrician, who quickly referred us for further testing. He ended up getting a dual scope—both a colonoscopy and an upper endoscopy (the technical term I had forgotten at the time)—to see what was going on inside.
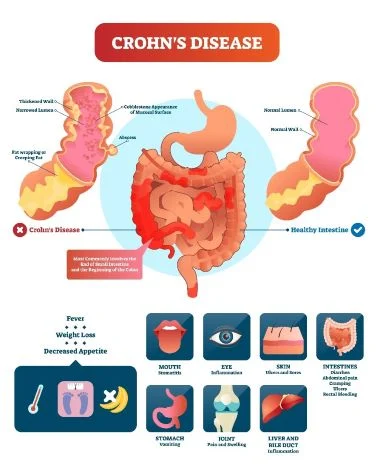
The results came back with a diagnosis we weren’t expecting: Crohn’s disease.
Crohn’s disease is a chronic inflammatory condition of the gastrointestinal tract. It’s part of a broader group of illnesses called inflammatory bowel disease (IBD). While some cases are hereditary, most are not. We had no family history. For us, this diagnosis seemed to come out of nowhere. But looking back, there were hints—his paleness, a lack of vitamin D from being inside all day, and a high-sugar, low-protein diet that probably didn’t help his gut health.
The Typical Approach for Crohn’s Disease
At our first meeting with the pediatric GI specialist, we were introduced to the standard treatment approach for Crohn’s disease: medication. Not just a pill or two, but long-term immunosuppressive drugs and biologic therapies like Remicade (infliximab) or Humira (adalimumab). These are usually administered via infusions every six to eight weeks—sitting with a needle in your arm for hours at a time. That didn’t sit well with my son. Like me, he hates needles.
To his credit, he asked a powerful question for a teenager: “Can I try managing it with diet instead?”
Our doctor didn’t say no, but she made it clear it would be tough—especially for someone his age. She didn’t think many kids could stick to a restricted diet for long enough to see a difference. But as she described what such a diet might look like, I was reminded of something I had just read: a book called The Plant Paradox.
A Different Path
I won’t dive deep into The Plant Paradox here (that’s a post for another day), but the core idea is that many foods—even so-called “healthy” ones—contain plant proteins like lectins that can irritate the gut and trigger inflammation. It’s not just about going gluten-free or cutting dairy; it’s about removing the foods that cause stress to your gut and slowly reintroducing safe options. Sounded a lot like what the doctor was suggesting.
My son was referred to a nutritionist, and to my surprise, the food list she provided mirrored the guidelines I had just read about in The Plant Paradox. So with support, he began a strict elimination diet, starting with the gentlest foods: cassava root, sweet potatoes, and other non-inflammatory options.
Rebuilding from the Inside Out
The early days were rough. He was eating very basic meals, but over time, he began reintroducing foods—just two new ones per week. He’d watch closely to see how his body responded. Some worked, some didn’t. Over time, he built up a personalized list of “safe” foods.
He eliminated gluten, dairy, and significantly reduced added sugars. (Side note: I didn’t realize just how bad added sugar is for gut health until this process—it’s incredibly inflammatory.) We learned to read labels carefully, avoiding additives like xanthan gum and sneaky sweeteners hiding in everything from kombucha to sauces.
With each week, his color came back. He gained weight—going from 108 up to 135 pounds. He built muscle, especially once he resumed cross-country training. And in a full-circle moment, he PR’d in the 5K during his senior year, clocking a blistering 16:30. That’s not just a win for his health—that’s elite-level high school running.
Medical Pressure and a Turning Point
Despite all this progress, the GI clinic kept pushing for medication. Their assumption was that he would eventually fail the diet approach, like most kids did. At one point, they told us they would refuse to continue care unless we agreed to begin biologics.
But we stood our ground. We asked for more time. We could see the improvements happening—weight gain, energy, color, strength. We asked to wait until the next round of labs.
And when the results came in… they were perfect.
Normal bloodwork. Normal stool samples. His C-reactive protein, which had been way out of range early on, was now back to healthy levels. The doctor sent a note through the portal saying his numbers were “amazing.” In person, she looked at us, remembered our conversation about The Plant Paradox, and asked if he had followed that protocol.
I smiled and said, “He didn’t listen to me. But he did listen to the nutritionist.” And since her list aligned almost exactly with what I had read, the answer was effectively: yes.
Five Years Later
Today, my son is 21. He continues to get regular checkups and will soon go in for a five-year scope to confirm everything still looks good. But to this day, he’s never gone on medication. No infusions. No injections. Just real, whole food.
He’s learned how to manage the occasional indulgence—yes, he still has a sweet tooth—and he understands how his body responds. He knows what to expect if he strays and how to recalibrate when he does. That level of self-awareness and discipline is something I admire deeply.
In fact, at a recent visit, his adult GI doctor (who also treats my wife) mentioned that my son is the only Crohn’s patient in his practice not on medication. Not because it’s impossible—but because very few people can stick to the kind of nutrition regimen my son has embraced.
The Bigger Picture
I’ve said this before, but it bears repeating: we live in a society that’s often more comfortable with treating symptoms than addressing root causes. Whether it’s Crohn’s, heart disease, or cancer, we default to medical interventions—many of them necessary, but often not the only option.
What my son’s journey showed me—what it showed him—is that the power of food is real. It can heal. It can transform. And in some cases, it can eliminate the need for prescription medication altogether.
We’ve adopted much of his diet into our own household—more whole foods, less sugar, fewer additives. We’re healthier for it, and incredibly proud of the path he’s walked.
If you or someone you love is facing a Crohn’s disease diagnosis, I hope this story offers a little hope—and maybe a different way forward.

Leave a Reply
You must be logged in to post a comment.